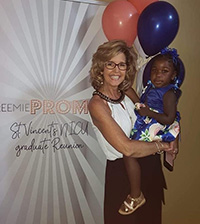
Lisa Costa grew up near Birmingham, Alabama, and has lived in the area her whole life. For more than twenty years, she has worked as a neonatal nurse practitioner at St. Vincent’s Hospital, one of the largest delivery hospitals in the state. Over the last several years, as the opioid crisis has become more prevalent in Alabama, her interest in substance-exposed babies has grown to a passion.
Lisa Costa grew up near Birmingham, Alabama, and has lived in the area her whole life. For more than twenty years, she has worked as a neonatal nurse practitioner at St. Vincent’s Hospital, one of the largest delivery hospitals in the state. Over the last several years, as the opioid crisis has become more prevalent in Alabama, her interest in substance-exposed babies has grown to a passion.
 “I attended a conference about how to better care for those infants, and then a physician and I rewrote all of our policies to reflect practices that would lead to better outcomes. That was at the beginning of the opioid crisis, and we kept getting more and more of these infants and realized it was a much bigger issue.” Lisa was asked to participate in the Alabama Substance Use in Pregnant Women and Neonatal Opiate Withdrawal Syndrome (NOWS) Task Force. The task force is a joint effort by the Alabama Department of Public Health and the American Academy of Pediatrics, and its membership includes physicians, nurse practitioners, pharmacists, and other experts. As a member of the task force’s protocol committee, Lisa works with other practitioners and experts to develop a toolkit with new protocols for caring for infants suffering from NOWS. As the opioid crisis grows, the task force is committed to disseminating the information they’ve learned with hospitals across Alabama.
“I attended a conference about how to better care for those infants, and then a physician and I rewrote all of our policies to reflect practices that would lead to better outcomes. That was at the beginning of the opioid crisis, and we kept getting more and more of these infants and realized it was a much bigger issue.” Lisa was asked to participate in the Alabama Substance Use in Pregnant Women and Neonatal Opiate Withdrawal Syndrome (NOWS) Task Force. The task force is a joint effort by the Alabama Department of Public Health and the American Academy of Pediatrics, and its membership includes physicians, nurse practitioners, pharmacists, and other experts. As a member of the task force’s protocol committee, Lisa works with other practitioners and experts to develop a toolkit with new protocols for caring for infants suffering from NOWS. As the opioid crisis grows, the task force is committed to disseminating the information they’ve learned with hospitals across Alabama.
 “I got to thinking that I might bring more value and influence to my role in that task force if I had the knowledge from an additional degree that would allow me to contribute further,” Lisa said. She had considered earning her doctorate for years, but this new opportunity to make a difference for infants and women across the state led her to pursue her Doctor of Nursing Practice (DNP), which she earned 100% online from The University of Alabama. Lisa’s own health concerns also motivated her to advance her education. “I want to stay in clinical practice for the rest of my career, but just in case my health issues prevent me from being able to do that, having my DNP gives me something to fall back on where I could teach at a higher level,” she explained.
“I got to thinking that I might bring more value and influence to my role in that task force if I had the knowledge from an additional degree that would allow me to contribute further,” Lisa said. She had considered earning her doctorate for years, but this new opportunity to make a difference for infants and women across the state led her to pursue her Doctor of Nursing Practice (DNP), which she earned 100% online from The University of Alabama. Lisa’s own health concerns also motivated her to advance her education. “I want to stay in clinical practice for the rest of my career, but just in case my health issues prevent me from being able to do that, having my DNP gives me something to fall back on where I could teach at a higher level,” she explained.
Lisa considered a few other online DNP programs around the state, but ultimately chose UA’s because of the flexibility it offered. “I had been out of school for over 20 years, and I was nervous about being able to manage a full-time course load along with my work. UA’s program was flexible enough that I could take my time with it and pursue it part time while I maintained my professional commitments.”
Since it had been so long since Lisa had been a student, she was worried about jumping into doctoral-level courses in Fall 2017. “My first course was Writing for Publication. I’d never really written anything for publication in my life and thought maybe I was barking up the wrong tree with this degree!” she joked. “But as I started writing, I realized how passionate I was about what I was doing – it came out in my writing.”
 Lisa also had concerns about lacking a sense of community by taking classes online instead of face to face, but she was surprised to find the opposite was true. “The faculty and staff did a really good job with making it more personal. I didn’t feel like I was just somebody. They also did a great job connecting us to each other. I made friends all over the country across many different disciplines and have continued to keep up with those friends.”
Lisa also had concerns about lacking a sense of community by taking classes online instead of face to face, but she was surprised to find the opposite was true. “The faculty and staff did a really good job with making it more personal. I didn’t feel like I was just somebody. They also did a great job connecting us to each other. I made friends all over the country across many different disciplines and have continued to keep up with those friends.”
Lisa gained a great deal from the program’s coursework. After working with a limited patient population in the NICU for many years, she found insights from other areas of nursing that grew her understanding of a broader application of the nursing profession. “I enjoyed the classes that talked about population health and health policy and politics. It all came together and opened my eyes to how much influence nurses have or can have if they want to be involved.”
 Her dissertation focused on improving substance abuse screening in obstetrics offices so health professionals can be proactive instead of reactive in caring for mothers and infants affected by opioid use. Lisa explained that many obstetricians in her area didn’t realize how pervasive the problem of opioid use is. “My project opened their eyes to see that they had this patient population in their offices. They just didn’t know they had patients with these issues because they weren’t asking.” Lisa’s project encouraged screening patients early in pregnancy in order to provide them the education and other resources or services they may need to better care for themselves and their babies.
Her dissertation focused on improving substance abuse screening in obstetrics offices so health professionals can be proactive instead of reactive in caring for mothers and infants affected by opioid use. Lisa explained that many obstetricians in her area didn’t realize how pervasive the problem of opioid use is. “My project opened their eyes to see that they had this patient population in their offices. They just didn’t know they had patients with these issues because they weren’t asking.” Lisa’s project encouraged screening patients early in pregnancy in order to provide them the education and other resources or services they may need to better care for themselves and their babies.
Lisa completed her dissertation and graduated with her DNP in May 2020. Earning the extra credentials behind her name has empowered her to have a greater influence for patients and communities, and she looks forward to seeing how having her DNP will continue to positively impact her career in the future.
“It made me a much more well-rounded nurse, and I’ve realized one person can make a much bigger change than they think they can.”
Published: September 30th, 2020